In our last blog, we covered the importance and utility of Rapid Antibody Testing, especially in COVID-19 hotspots. However, it is important to understand the limitations of this test and that it cannot be used as a substitute for diagnosing COVID-19. It makes screening of suspected cases easier and assessing immunity to virus possible BUT it doesn’t replace the confirmatory diagnosis of COVID-19 provided by Real Time Reverse Transcription Polymerase Chain Reaction (RT-PCR) test, mandated by WHO.
Let’s have a look at the limitations and challenges of Rapid Antibody Tests
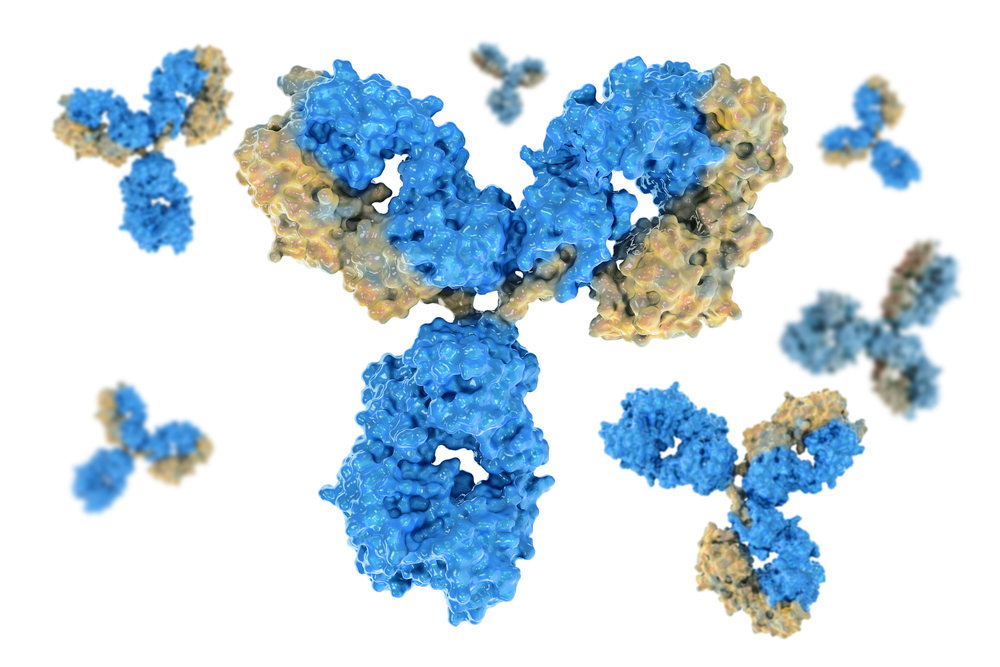
- Body’s antibody response to COVID-19 is relatively slower than usually expected. While supporting data is limited at this point, it has been observed that the initial IgM antibody response doesn’t peak until 9 days after initial infection and the IgG antibody response doesn’t peak until day 11, whereas most viruses take 5 days to produce initial immune response.
- Rapid test can ensure the immunity of people but cannot provide the information that would confirm that they are no longer carriers of the virus. For that purpose, RT-PCR plays an important role.
- It may give false negative results – if done in the window period before the antibody appears in the system [antibody takes 8-14 days to develop following natural infection]
- Technical challenges in making antigens: Difficult to make the protein in laboratories using cell cultures which forms the viral coat, essential to trigger the immune response to produce antibodies for inclusion in immunoassays. There are questions which antigens [proteins] are the best to produce antibodies
- Nucleocapsid protein: the most abundant viral protein, which means it’s easy to detect, but less specific
- Spike protein: more specific, more divergent but which part of it to be used is less obvious
- False positive results: due to cross reactivity to other coronavirus infections; amino acids of the spike proteins of SARS and the COVID-19 virus, there’s a 75% identity and overall figure for common cold-causing coronaviruses is probably about 50–60%.