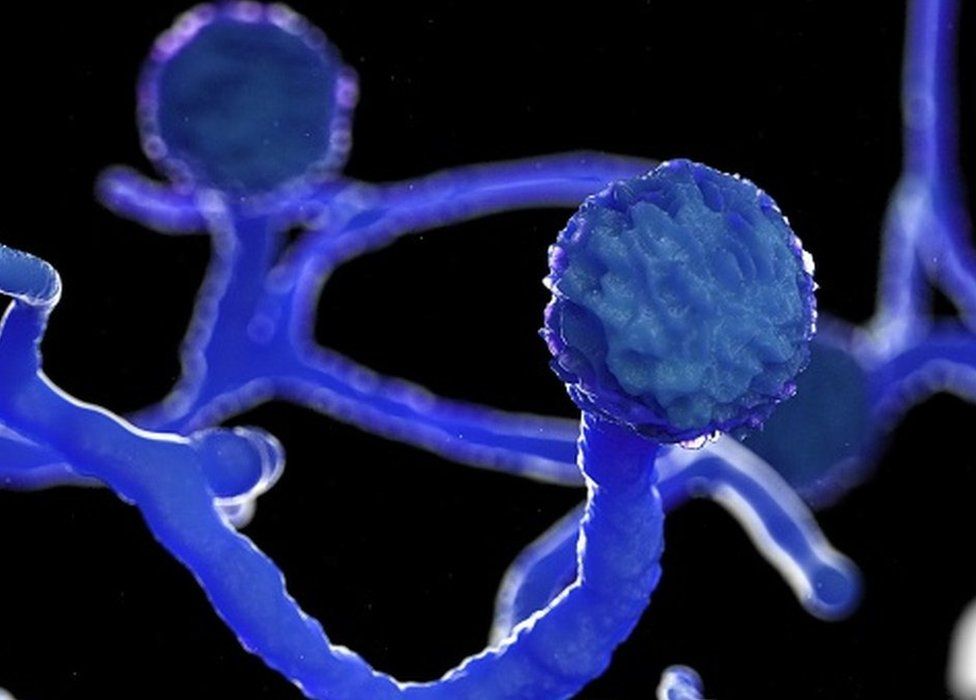
What is Mucormycosis?
Mucormycosis is a disease that is caused by fungal organisms that belong to the order Mucorela. Among the various fungi, the species called Rhizopus is the most common. Other fungi that can cause this disease includes Mucor, Apophysomyces, Cunninghamella, Lichtheimia, Saksenaea, Rhizomucor etc. Infections with this group of fungi can be life-threatening and must be diagnosed and treated aggressively at the earliest, before it spreads to the surrounding tissues and the brain.
It is commonly seen in patients who have developed complications of diabetes like diabetic ketoacidosis, have compromised immune systems and in patients who have a low neutrophil (a type of white blood cell) count especially in those taking treatment for cancer.
Why is it appearing now in India?
Mucormycosis is commonly seen in diabetics (uncontrolled) and in individuals who have their immune system suppressed, either due to any disease or taking medication that suppresses the immune system e.g. Steroids, anticancer medication etc.
During the COVID 19 pandemic there are several patients who have been on steroids for a long duration and that coupled with uncontrolled diabetes can be a conducive environment for this fungal infection. Also high ferritin could encourage the growth of this infection.
How is it diagnosed?
The disease can be diagnosed by tissue biopsy which can be observed by histopathological examination. Some tissue can be viewed immediately under the microscope using the Potassium Hydroxide fluid to check for the presence of fungal filaments. In addition, fungal culture can be done from the tissue to grow and detect the type of fungus. CT scans are done to detect the extent of spread of the infection and check for the amount of tissue destruction.
Mucormycosis symptoms
The disease can present with blockage of one of the nostrils, black discoloration over the nasal area, pain and or numbness in sinus region, redness and swelling of the sinus region, black discharge from the nose, one sided headache, toothache and loosening of teeth, double vision (when it spreads to the eye regions). If the fungus spreads to the lower respiratory system, it may also lead to coughing blood and breathlessness or shortness of breath.
In case fungal spores are ingested it can give rise to gastrointestinal symptoms in those who are malnourished. On inhalation, the fungal spores are deposited in the nasal turbinates and then begin to spread from there by invading and destroying the surrounding tissues
How is it prevented and treated?
Treatment involves management of the underlying risk factors like diabetes, steroid/cancer therapy, starting antifungal medication like Amphotericin B and surgical debridement of the affected area
Can mucormycosis be cured?
Mucormycosis can be managed if early diagnosis and treatment is initiated. This is essential as the disease has a high mortality rate
Which are common locations of mucormycosis?
The nose, paranasal sinuses, orbital region (eye), brain, respiratory, gastrointestinal system, skin can be affected by Mucormycosis
Who is at risk for mucormycosis?
Those with uncontrolled diabetes with complications
Those with suppressed immune systems due to drugs like steroids or chemotherapeutic drugs for cancers
Is mucormycosis serious?
Mucomycosis can be life threatening and must be diagnosed at the earliest. Treatment requires medical therapy along with surgical debridement and removal of the affected dead tissue by surgery. The mortality rate from Rhinocerebral (affected nasal region and brain) Mucormycosis is about 50-75%
Is mucormycosis airborne?
The spores of Mucor group of fungi are ubiquitous, that is they are present everywhere especially in the soil and decaying matter. Inhalation or ingestion of these spores, in those whose immune systems are compromised may lead to the disease.
For more information on Mucormycosis, read the study conducted here
If you would like more information on testing for Mucormycosis, read about our testing options here